Quest for Excellence is our vision of creating exceptional patient experiences through continuous improvement. Our institutional challenge is “to be better tomorrow than we are today!”
We strive to provide the best patient care in a safe and efficient environment. We work towards this goal every day through continuous process improvement, leadership development, using lean methodology. As a resident in our program, you will have the opportunity to integrate your clinical education into a culture of excellence in quality and safety that is designed for physician leaders.
Quest for Excellence is closely aligned with the CLER Pathways to Excellence. Quest has four areas of focus designed to help us along our continuous improvement journey. These interdependent areas of focus include:
CLER Pathways to Excellence
NGMC is one of a handful of sponsoring institutions created after the ACGME developed its CLER Pathways to Excellence. These pathways are seen by the ACGME as essential to creating an optimal learning environment.
The CLER Pathways include six focus areas: patient safety, health care quality, care transitions, supervision, well-being, and professionalism. There are multiple pathways in each of the focus areas, and each pathway includes key properties that can be used for assessment at the institutional level.
The Importance of Patient Safety & Quality (PS&Q)
NGMC is dedicated to building Safety CHAMPS in healthcare. That said, there are numerous ways that safety and quality can be impacted. Wellness, fatigue, unwillingness to ask questions, or even not having the willingness to speak up, can all lead to increased risk which result in potential safety incidents and/or errors.
Our program of “Building Safety CHAMPS” has a goal of ZERO preventable harm.
- Communicate Clearly
- Handoff Effectively
- Act with a Questioning Attitude
- Maintain Your Wingman at All Times
- Pay Attention to Detail
- Speak Up for Safety
Patient Safety and Quality are monthly topics as a part of our Cornerstones of Resident Education (CORE) curriculum.
“A culture of safety requires continuous identification of vulnerabilities and a willingness to transparently deal with them. An effective organization has formal mechanisms to assess the knowledge, skills, and attitudes of its personnel toward safety in order to identify areas for improvement.”
– Quote from the ACGME –
Leadership Development
In most residency training programs, the focus is mostly (or wholly) on clinical skill development. At NGMC, we believe that leadership development is also a skill that must be developed.
Our curriculum is structured around three major competencies: personal authenticity, interpersonal effectiveness and continuous improvement. This leadership development model includes emotional intelligence and professional competence; effective communication and building trust; and vision, innovation and change management.
Error Prevention Toolkit
We have also developed an Error Prevention Toolkit (EPT) training program for leaders and front-line staff to ensure that we are moving forward with our safety initiatives using existing infrastructure, and not creating another system. The EPT training course was first rolled out in 2016 and is now required for all employees and physicians. Our entire Medical Staff has been trained! Each month, we focus on a different safety tool and safety behavior.
Learning from Toyota
The primary task of Toyota’s managers and leaders does not revolve around improvement…but around increasing the improvement capability of people. That capability is what, in Toyota’s view, strengthens the company.”
– Mike Rother, Toyota Kata –
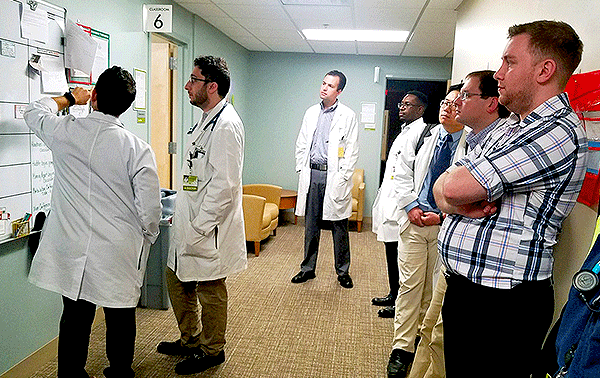
Daily Management System
Every day in the modern healthcare system, we deal with unavailable supplies, missing information, broken equipment, difficult to follow procedures and other barriers to providing efficient and effective care. In most systems, we develop workarounds and put out fires, but we never seem to solve the problem. Over time, these problems become the norm.
One of the methods we address this in our system is our daily management system which consists of tiered huddles. These huddles provide an opportunity for staff to identify and work through problems that get in the way of patient safety. At each of the 410 huddles that occur across the system, teams determine the readiness for delivering safe and effective patient care, efficient use of resources, and good patient flow.