CSI nominated for prestigious SSH DAISY team award in healthcare simulation

The Center for Simulation and Innovation (CSI) team has been nominated for the Society for Simulation in Healthcare (SSH) DAISY Team Award, recognizing their extraordinary impact on maternal healthcare education and patient safety. The CSI team has confronted Georgia’s maternal healthcare crisis head-on through innovative simulation-based training that directly translates into saved lives. Their work includes establishing regional maternal emergency protocols through partnerships with the Georgia Perinatal Quality Collaborative and HOPE for Georgia Moms, delivering educational content selected for national distribution by AWHONN, and providing the opening simulation for the first annual Maternal Cardiac Roundtable. The team’s mobile simulation program has brought critical training to 11 rural communities and 15 EMS services across northeast Georgia, many in designated maternity care deserts, while their in-situ training model ensures that clinical teams are prepared for real-world obstetric emergencies.
Through their commitment to excellence, compassion and innovation, the CSI team has positioned NGHS among only 34 hospitals nationally recognized for simulation excellence, achieving both ASPE Full Accreditation and SSH accreditation in teaching and education. Their nurse-led approach demonstrates that simulation education extends far beyond the simulation lab, it creates a culture of readiness, vigilance, and advocacy that transforms healthcare providers into life-saving champions for their patients and communities.
Family Medicine residents blend celebration with hands-on clinical training

In November, Family Medicine residents gathered for a holiday potluck before transitioning to an afternoon of comprehensive simulation-based learning that combined didactics, hands-on workshops and immersive clinical scenarios. The training included managing complications in a post-operative colectomy patient, with both patient and family members incorporated into debriefs to strengthen communication skills and refine care strategies. Residents advanced their technical abilities by refining suturing techniques under Dr. Hogue’s guidance and enhancing their point-of-care ultrasound (POCUS) skills with Dr. Klas. The session concluded with an interactive escape-room challenge facilitated by hospital sepsis program navigators, where residents reinforced critical sepsis management principles through a competitive, team-based exercise that promoted collaboration and rapid clinical decision-making. This multifaceted approach to resident education demonstrates the program’s commitment to developing both technical proficiency and the essential communication skills required for comprehensive family medicine practice.
Tallulah Falls School students experience real-world healthcare training through mobile simulation lab

Health occupation students at Tallulah Falls School gained invaluable hands-on medical training when CSI’s Mobile Simulation Lab arrived on campus, transforming learning into an immersive real-world experience. Throughout the day, students engaged in high-stakes medical scenarios that challenged them to apply critical healthcare skills, including delivering a baby, mastering Stop the Bleed techniques for emergency hemorrhage control and performing comprehensive patient assessments using Pedi Hal, a sophisticated pediatric manikin. The young aspiring healthcare professionals also practiced administering life-saving epinephrine injections for anaphylactic emergencies, gaining the kind of practical experience that textbooks alone cannot provide. This dynamic training opportunity not only equipped students with essential technical skills but also built their confidence and prepared them for careers that await them in the healthcare field.
Emergency Medicine residents sharpen skills through simulation and game-based learning
Emergency Medicine residents participate in comprehensive monthly simulation training designed to build both technical proficiency and communication skills under pressure. High-acuity scenarios included traumatic cardiac tamponade, splenic rupture, pediatric status epilepticus with a distressed parent and thyroid storm in an anxious patient. PGY-3 residents engaged in advanced communication simulations focused on delivering difficult news to grieving family members. Supporting these clinical scenarios, Dr. Johnson provided hands-on education on the Blakemore tube—a critical intervention for uncontrolled upper gastrointestinal bleeding—and Dr. Hogue delivered instruction on epistaxis management and foreign body removal.
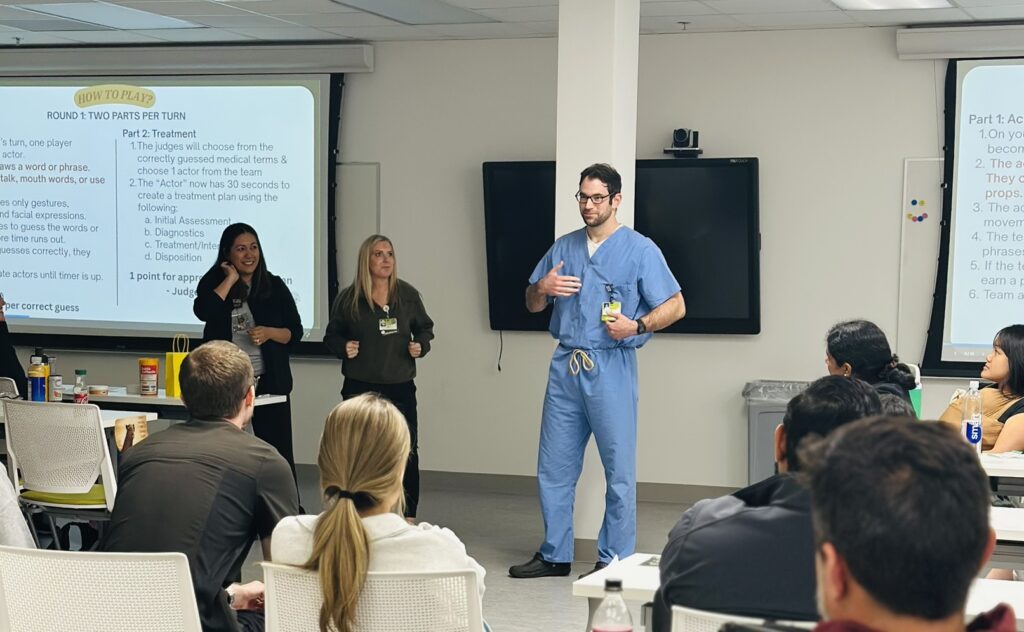
Building on this foundation, PGY-2 and PGY-1 residents recently participated in “Side Effects: Medical Charades,” a fast-paced competition that blends clinical reasoning with active learning. Teams of four competed under the guidance of PGY-3 chief residents Dr. Cranston and Dr. Rahhal, who served as judges. Each round challenged players to act out a diagnosis under time pressure, followed by a rapid-fire clinical summary where one teammate had thirty seconds to outline the initial assessment, key diagnostics, working diagnosis and likely disposition for a judge-selected case. This approach leverages game-based learning theory, which demonstrates that competition, movement, and time-limited decision-making enhance engagement, recall and knowledge application. For emergency medicine residents facing high-stakes board exams and real-time clinical demands, these combined training methods reinforce pattern recognition, communication and critical thinking in memorable and effective ways.
Rapid response team (RRT) training enhances resident emergency response skills

This November marked the successful completion of RRT simulations, all carefully reviewed and revised to reflect current policy changes and best practices. Internal medicine residents participated in comprehensive simulation scenarios including acute coronary syndrome with code blue, respiratory failure requiring intubation, ischemic stroke and stroke with hemorrhagic conversion. To further strengthen their clinical capabilities, residents also engaged in a dedicated airway workshop that provided crucial hands-on practice complementing the respiratory failure case scenarios. The training proved highly valuable, with residents enthusiastically embracing the challenges and gaining essential pearls of wisdom on effectively leading RRT responses, stroke alerts and STEMI alerts. The program’s success was made possible through the outstanding contributions of critical care nurses, RRT and respiratory therapists whose expert participation and dedication created an authentic and impactful learning environment for all involved.
Learn more
Learn more about the Center for Simulation and Innovation at NGMC.
